“We give you the right care in the right place, at the right time, by the right person.”
We are part of Walsall East 2 Primary Care Network.
Complaints Policy & Procedure
Policy Statement
At The Oaks Medical Centre & Blackwood Health Centre, we take all complaints seriously. We are committed to ensuring all patients and staff understand their right to have complaints acknowledged and thoroughly investigated. We will ensure that complaints are handled in a fair, transparent, and timely manner, keeping the complainant informed throughout the process.
Status
This document outlines the complaints policy for The Oaks Medical Centre & Blackwood Health Centre. It is non-contractual and may be revised at any time. It applies to all staff, including employees, locums, agency workers, and contractors. The organisation ensures that no one is disadvantaged when making a complaint, in line with the Equality Act 2010.
Complaints Management Team
The Complaints Officer for The Oaks & Blackwood is Jodie Byrne, who is responsible for triaging and managing all complaints, both clinical and non-clinical. The following individuals are also nominated as Responsible Persons for ensuring compliance:
- Jodie Byrne
- Dr. Anne Lewis
They will ensure action is taken where necessary, following the complaint investigation outcome.
Complaint vs. Concern
A concern is a worry or issue that can often be resolved informally, while a complaint is a formal statement about dissatisfaction that requires a response. If a concern cannot be resolved at the time it is raised, it may escalate into a formal complaint.
Formal or Informal Complaints
Complaints can be either formal or informal. If a matter can be resolved quickly, the Complaints Officer may classify it as an informal concern. If it requires further investigation, it will be logged as a formal complaint. Complaints made verbally should still be documented, especially if not resolved within 24 hours.
Complaints Information
We ensure that patients are aware of how to make a complaint by providing clear information through:
- Notices displayed within the practice
- Information on the website
- Complaints leaflets available at reception
Duty of Candour
We are committed to being open and transparent with patients, particularly when things go wrong. This is in line with both the statutory Duty of Candour and professional duties, ensuring patients and their families are informed when there are concerns.
Role of the Parliamentary and Health Service Ombudsman (PHSO)
If a complaint is not resolved locally, the PHSO may be involved to review the case and recommend actions, including apologies, explanations, and financial remedies.
Complaints Procedure – Steps for Complainants
- Stage 1: The patient or their representative can make a complaint directly to us or to the Integrated Care Board (ICB). See information on last page.
- Stage 2: If the complainant is dissatisfied with the outcome, they can escalate the complaint to the PHSO. See information on last page.
Timescale for making a Complaint
A complaint must be made within 12 months of the incident or from when the complainant becomes aware of the issue. In some cases, complaints made after this time frame may still be considered if there are reasonable grounds for the delay.
Responding to Complaints
We aim to respond to all complaints within the following timeframes:
- Immediate response: If the complaint can be resolved on the spot, this should be done. If necessary, move to a quieter space to discuss further.
- Formal response: The Complaints Officer will acknowledge receipt of a formal complaint within three working days. A full investigation will be carried out, with updates provided if needed with a response within three months.
Verbal Complaints
If a complaint is raised verbally and resolved immediately, it may not need to be logged formally. However, any verbal complaint not resolved within 24 hours will be recorded in the Complaints Log.
Written Complaints
All written complaints will be fully investigated, and a written response will be provided, including details of the investigation and any actions taken.
Who Can Complain?
Complaints can be made by:
- The patient
- A person acting on the patient’s behalf, however this can only be completed with written and signed consent from the patient.
- A child’s representative (in the child’s best interest)
- The personal representative of a deceased person
- Someone with the patient’s consent (including legal representatives like Power of Attorney)
Complaints Advocates
Patients have access to independent NHS complaints advocates. Information on how to contact an advocate can be found in the complaints leaflet and on our website. Local Healthwatch may also help find independent advocacy services.
Investigating Complaints
We will investigate all complaints in a fair and thorough manner, ensuring transparency and objectivity. The process includes:
- Assigning a lead investigator
- Reviewing all facts and evidence
- Ensuring the complainant is kept informed throughout the investigation
Confidentiality
All complaints will be treated confidentially, and information related to the complaint will be stored separately from the patient’s medical records.
Persistent and Unreasonable Complaints
We follow a Zero Tolerance Policy for persistent or unreasonable complaints. If a complaint is persistent or vexatious, guidance will be sought from the ICB before responding.
Complaints Involving Legal Action
If a complaint mentions potential legal action, the Complaints Officer will consult with the relevant defence union for guidance before responding. If the complaint relates to clinical matters after 1 April 2019, NHS Resolution may assist under the Clinical Negligence Scheme for General Practice.
Complaints about External Staff
If a complaint involves external staff (e.g., locum workers), we will inform the relevant organisation’s Complaints Manager and collaborate to resolve the issue.
Fitness to Practice
If a complaint is of a clinical nature and raises concerns about a clinician’s fitness to practice, the Senior Partner will review the case and, if necessary, refer it to the relevant professional body.
Learning from complaints
All complaints are discussed confidentially at practice meetings to ensure that all learning from the complaint is shared with the relevant staff.
Logging and Tracking Complaints
All complaints will be logged and tracked to identify trends or areas for improvement. We will monitor the process closely to ensure timely responses and proper resolution.
Use of complaints as part of the revalidation process
Outlined processes
As part of the revalidation process, GPs must declare and reflect on any formal complaints about them in tandem with any complaints received outside of formal complaint procedures at their appraisal for revalidation. These complaints may provide useful learning.
The following information is to support the appraisal and revalidation process for various healthcare professionals:
| GPs | Royal College of General Practitioners (RCGP) |
| Nurses | Nursing and Midwifery Council (NMC) |
| Pharmacists | General Pharmaceutical Council (GPhC) |
| Other healthcare professionals | Healthcare Professionals Council (HCPC) For Physician Associates, refer to the Royal College of Physicians |
Final Response
Once the investigation is complete, the complainant will receive a final written response within three months. If the investigation takes longer, we will inform the complainant and provide a timeline for completion.
If you do not want to complaint directly to the surgery you can contact:
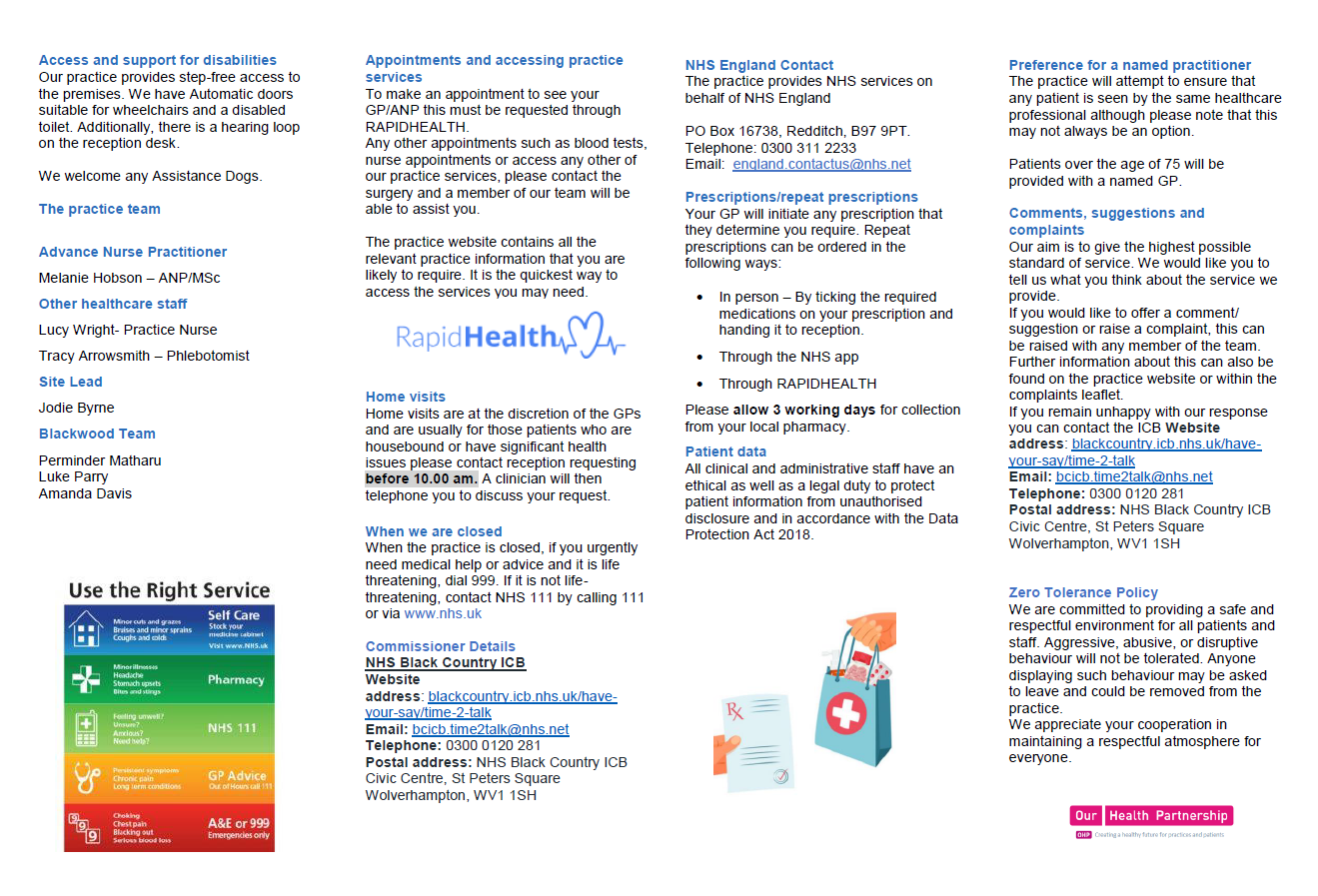
Integrated Care Board (ICB)
Write to: Time2Talk Team, Black Country ICB, Civic Centre, St Peters Square, Wolverhampton, WV1 1SH
Email for complaints: bcicb.time2talk@nhs.net
Call: 0300 0120 281
Website: www.blackcountry.icb.nhs.uk/have-your-say/time-2-talk
If you are unhappy with the response from the ICB/Practice please see below:
Parliamentary and Health Service (PHSO) Ombudsman If you are not happy with the outcome of your complaint, you can contact the Parliamentary and Health Service Ombudsman (PHSO) free of charge. They can review the way in which your complaint has been handled, but you will need to contact the Ombudsman about your case within 12 months of the final local outcome of your complaint.
Email: PHSO.enquries@ombudsman.org.uk
Telephone: 0345 015 4033
Website: www.ombudsman.org.uk